By David Evans and Katrina Kosec
A whirlwind, surely incomplete tour of cash transfer impacts on health
Your run-of-the-mill conditional cash transfer (CCT) program has significant impacts on health-seeking behavior. Specifically, there are conditions (or co-responsibilities, if you prefer) that children get to school and/or that they get vaccinated or have some wellness visits. While the school enrollment effects are well established, the effects on both health seeking behavior and on health outcomes have been much more mixed. CCTs have led to better child nutritional status and improved child cognitive development in Nicaragua, better nutritional outcomes for a subset of children in Colombia, and had no impacts for child health in studies on Brazil and Honduras. CCTs conditioned only on school enrollment did not lower HIV infections among adolescent girls in South Africa; and in Indonesia CCTs increased health visits but did not translate into measurably improved health. Unconditional cash transfer programs have also had mixed results on health, with better mental health and food consumption in Kenya, better anthropometric outcomes for girls (not boys) in South Africa, no average impacts (although some for the poorest quarter) on child outcomes in Ecuador, and no average impacts on maternal health care utilization in Zambia (albeit yes effects for women with better access to such services).
Only a few studies have explicitly compared health impacts of programs with and without conditions. In Burkina Faso, CCTs increased preventative health care visits but UCTs did not. In Zimbabwe, there weren’t clear differences. In Malawi, UCTs lowered teen pregnancy over CCTs, and a later study suggests better mental health impacts of UCTs.
(Of course, there are cash transfer that specifically condition on health, such as those to prevent sexually transmitted diseases. You can read about those elsewhere – say, here and here.)
New evidence on cash transfers and health: Not just what they do, but when and how
In a new paper with Brian Holtemeyer, we evaluate the impact of conditional cash transfers on health seeking behaviors and health outcomes in Tanzania. The program provided $3 per child and $6 per elderly to vulnerable households, conditioned on health clinic visits every other month for children 0-5, annual health clinic visits for the elderly, and school enrollment and 80 percent attendance for older children. We followed up with households both 1.5 years and 2.5 years after initiation of transfers. (Before we leap into discussing an array of results, we correct for multiple hypothesis testing in three ways and the results generally hold up.)
Here is what we learned:
1. Measure at the right time: We observe no average change in health at 1.5 years. But by 2.5 years out, we observe that sick days were reduced. Specifically, for our whole treatment group, the probability of having been sick in the last month fell by about 4.5 percentage points (17 percent), and sick days fell by half a day (27 percent decrease). This is mostly driven by improvements for children age 0-5, for whom the drop in probability of illness is more than 10 percentage points, and the reduction in days sick is 0.76.
But why don’t the impacts show up after 1.5 years? Digging into the data reveals that in fact, there were reductions in illness for a subset of the population. As you can see in the figure below, at 1.5 years (“midline”), those who were already attending the clinic regularly – even before the transfers began –were experiencing gains relative to the control group, suggesting an income effect (rather than an incentive effect) on health. But by 2.5 years (“endline”), the impacts had reversed, showing larger health impacts for those that the program drew to the clinics.
2. Don’t underestimate the power of messaging: At first glance, we see a rise in health clinic visits at 1.5 years, but that effect mysteriously disappears by 2.5 years. Why? With more detailed analysis, we see that 60 percent of households were already complying with visits at baseline. It may be that the introduction of the program made visiting the clinic more salient, increasing visits even among those who were already exceeding the conditions. Over time, as understanding of the program increased, those households may have reduced their visits to only those actually required. (There are other possible explanations for the dissipation of this effect: For example it looks like control villages raised their visits by endline, perhaps in anticipation of the expected rollout of the program to them.)
3. Supply side matters: While the effect of receiving transfers wasn’t significantly affected by the baseline health workers per capita at local clinics, the health impacts were. In the villages with more staff, the reduction in sick days in the last month was 0.96, whereas the number was 0.07 in poorly staffed villages. As you can see in the figure below, by endline, sick days are lower relative to control villages at all levels of staffing, but the biggest effects (and the significant ones) are in villages with well-staffed clinics.
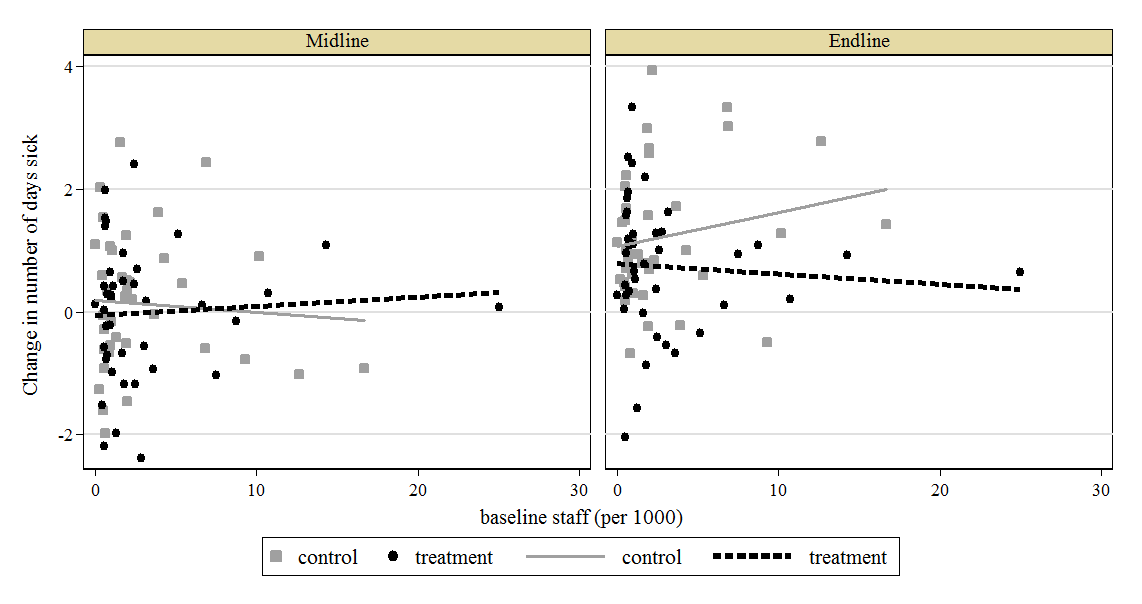
In other words, cash transfers don’t work in a vacuum, and the health effects are likely to be biggest when the health care system has the capacity to respond to the increased demand associated with the program.
4. People want to shield themselves from risk: We see big gains in participation in the most widespread form of local health insurance, the Community Health Fund (CHF). Household reported expenditure on insurance rose by six times at midline and eight times at endline. By endline, treatment households were 36 percentage points more likely to be enrolled in the CHF than were control households. We also observe sizeable reductions in households financing health expenditures with cash, instead using health insurance to finance treatment. As far as we know, this is the first cash transfer evaluation to examine the impact on take-up of insurance, and the effects are striking.
Takeaway: Cash transfer programs are widespread, and they continue to expand. But as we continue to evaluate these programs, it’s crucial to measure impacts over a sufficient period to pick up those changes that are a cumulative result of many household decisions, like health. It’s also crucial to make sure that the supply side structures are in place to meet local demand; indeed new evidence from Indonesia points to how cash transfers can actually increase the supply of health workers. Program implementers need to help people understand the program conditions if there are conditions. And these results suggest that these transfers can not only increase incomes, but also shield the most vulnerable households from those most debilitating of shocks—those to health.
David Evans is a Senior Economist on the team for the World Bank’s 2018 World Development Report; Katrina Kosec is a Senior Research Fellow in IFPRI’s Development Strategy and Governance Division. This post also appears on the World Bank Development Impact blog.