Globally, 49 million children suffer from acute malnutrition, also referred to as wasting (weight-for length Z-scores (WLZ) < -2). Acute malnutrition kills 875,000 children under the age of five annually.
The Community-based Management of Acute Malnutrition (CMAM), endorsed by the World Health Organization, is a life-saving strategy that allows treating children suffering from severe acute malnutrition (WLZ<-3) without medical complications at the community level through an outpatient program. The effectiveness of CMAM programs, however, is limited due to low participation in screening and low uptake and adherence to treatment.
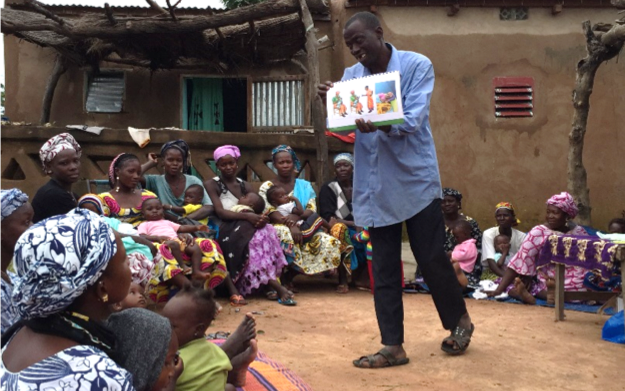
The Innovative Approaches for the Prevention of Childhood Malnutrition (PROMIS) program sought to overcome key barriers to CMAM effectiveness by integrating two preventive interventions into screening for acute malnutrition: (1) behavior change communication (BCC) on essential actions to improve child nutrition and health-seeking behavior; and (2) the provision of a small-quantity lipid-based nutrient supplement (SQ-LNS) to all children to increase intake of essential nutrients and prevent undernutrition. The overall goal was to test and evaluate the integrated model’s impact on:
- participation in screening—and referral, uptake of, and adherence to treatment;
- the prevalence and incidence of acute malnutrition;
- infant and young child feeding practices and appropriate use of SQ-LNS; and
- child linear growth and anemia.
The program was implemented by Helen Keller International in Burkina Faso, Mali, and Senegal between 2014 and 2017. IFPRI conducted a cluster-randomized trial in Burkina Faso and Mali to assess the program’s impact. In both countries, clusters (health centers) were randomly allocated to either the PROMIS program (treatment) or the national program (control). BCC and the distribution of SQ-LNS were done monthly at the time of screening for acute malnutrition, and children identified as being acutely malnourished were referred to treatment. In Mali, PROMIS was implemented through a community-based delivery platform, whereas in Burkina Faso, the program used a facility-based delivery platform (well-baby consultations). Details regarding the intervention and evaluation designs and key results are summarized here.