This post is the second in a series on a research project in Guatemala and Burundi that evaluated how to optimize food assistance programs for the maximum impact. Read the first here, second here, third here, fourth here, fifth here, and sixth here.
Evidence shows that food-assisted maternal and child health and nutrition (FA-MCHN) programs that target mothers and children during the first 1,000 days of life (from pregnancy to a child’s second birthday) succeed in achieving nutrition improvements. What are the effects of such programs on anemia (i.e., low hemoglobin levels), specifically, in mothers and children?
Women and children in the first 1,000 days are at particular risk of anemia. Anemia during pregnancy increases the chance of maternal mortality and has been associated with increased perinatal mortality, low birth weight, and, when caused by iron deficiency, delays in child development. Developmental delays, in turn, can have lifelong consequences, as they hinder cognitive development, school performance, employment, and accumulation of wealth.
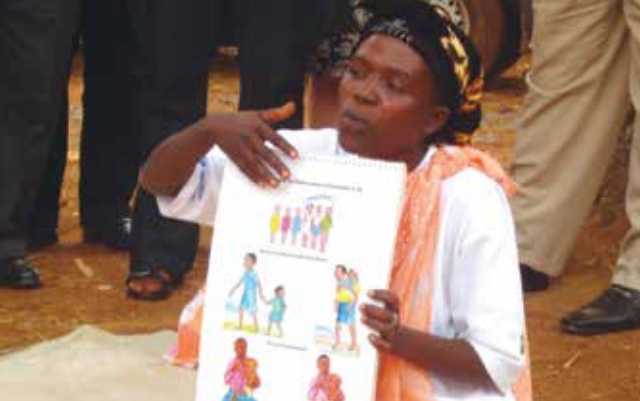
Certain components of FA-MCHN programs may help to reduce anemia, including the distribution of micronutrient-fortified commodities, behavior change communication (BCC) strategies around optimal child feeding and hygiene and health practices (for example, promoting the use of bed-nets to prevent malaria, an important cause of anemia), and the strengthening of health services.
The Tubaramure Program
Between 2009 and 2014, a consortium of NGOs led by Catholic Relief Services implemented a large-scale FA-MCHN program called Tubaramure (“let’s help them grow” in Kirundi) in eastern Burundi. The core program package included three key components: 1) the distribution of micronutrient-fortified food rations (corn-soy blend, or CSB, and fortified vegetable oil); 2) activities to strengthen health services; and 3) a BCC strategy focused on improving health, hygiene, and nutrition practices. All pregnant women and mothers with children under 6 months old were invited to participate in the program. They were encouraged to stay in the program until their children were 24 months old and, in the case of BCC activities, beyond.
Evaluating the Impact
To assess the program’s impact on maternal and child anemia and hemoglobin, IFPRI researchers Jef Leroy, Deanna Olney, Marie Ruel and colleagues carried out a randomized controlled effectiveness trial. In addition to evaluating the impact of the Tubaramure program, the study also evaluated possible impact pathways.
For the study, communities were randomly assigned to one of four treatment arms that included a control group and otherwise varied by the timing and duration of food-ration provision. Program impact was assessed through community fixed-effects double-difference models with repeated cross-sectional data (baseline and follow-up 2 years later). The program’s impact on hemogloblin and anemia was assessed by pooling the treatment groups.
To explore the possible impact pathways, the study used a two-step approach. IFPRI researchers began by estimating the impact on all the determinants of hemoglobin and anemia addressed by Tubaramure program activities.
- For children, these were CSB consumption, dietary diversity, consumption of iron-rich foods, minimum number of meals per day, bed-net use, and morbidity.
- For mothers, these were prenatal maternal iron-folate supplement and bed-net use, CSB consumption, dietary diversity, consumption of iron-rich foods, and postnatal bed-net use.
The researchers then tested the association between these determinants and anemia and hemoglobin levels to assess the plausibility that impact derived from each of these determinants.
Findings
This study is the first to show that a food-assisted MCHN program had positive effects on anemia and hemoglobin in both mothers and children. Children in the intervention groups experienced less of a decrease in hemoglobin and less of an increase in anemia compared with members of the control group, indicating that the Tubaramure program had a significant protective effect.
Though no overall program effect was found among mothers, significant protective effects on both hemoglobin and anemia were found among mothers who had given birth within the 3 months preceding the survey.
The study’s pathway analyses suggest that the positive effects of the program on child hemoglobin derived from improved dietary diversity, consumption of iron-rich foods, lower morbidity, and decreased fever; and on maternal anemia from dietary diversity, consumption of iron-rich foods, and bed-net use. Behavior change communications activities that promoted bed-net use were particularly successful in creating a massive increase in bed-net use among pregnant participants.
The findings demonstrate how development assistance in the form of FA-MCHN programs can play an important role in protecting poor families from economic or health shocks in vulnerable countries such as Burundi.
Jef Leroy is a Senior Research Fellow with IFPRI’s Poverty, Health, and Nutrition Division (PHND); Deanna Olney is a PHND Senior Research Fellow; Marie Ruel is Director of PHND; Tracy Brown is an IFPRI Senior Editor. This blog post is based on a project made possible by support from the United States Agency for International Development, the Food and Nutrition Technical Assistance III Project (FANTA) managed by FHI 360, and the CGIAR Research Program on Agriculture for Nutrition and Health.